Orlando’s Clinic for
BRAIN INJURY REHABILITATION
The aftermath of a brain injury is devastating, painful, and stressful. Your life and the lives of your loved ones are forever changed, but our proven treatment approaches will help you restore normal movement patterns, regain your independence, and get back to living your normal life again. Contact our expert brain injury specialist to schedule your appointment or read below to learn more about our stroke recovery services.
Orlando’s Clinic for
Brain Injury Rehabilitation
The aftermath of a brain injury is devastating, painful, and stressful. Your life and the lives of your loved ones are forever changed, but our proven treatment approaches will help you get back to living your normal life, regain your independence, and becoming pain-free again. Contact our expert brain injury recovery doctor to schedule your appointment or read below to learn more about our traumatic brain injury rehabilitation services.
Check out our latest education video!

Board-Certified
MEET DR. TARA TOBIAS
Dr. Tara Tobias is a board-certified neurologic physical therapy specialist. With 15+ years of experience, Tara has practiced in every setting including acute care, inpatient rehabilitation and outpatient centers that specialize in a variety of neurologic and balance conditions. Along with this, she has also completed numerous post-graduate courses focusing on the study of neuroplasticity (how the brain learns new skills and forms new connections), motor recovery, and the treatment of balance disorders.
The Two DifferentTypes of Brain Injury
Not every brain injury is the same, so it’s important to have a physical therapist that understands the different types, how they affect your body, and how you can best recover from it.
Traumatic Brain Injury
A traumatic brain injury is when there is damage to the nerves in the brain as a result of direct impact to the head. Often times referred to as a TBI, this type of brain injury disrupts the brain’s ability to function properly. You can learn more about traumatic brain injury here.
Hypoxic and/or Anoxic Brain Injury
Hypoxic and anoxic brain injury occurs when the brain is deprived of oxygen. Without the needed oxygen, nerves in the brain are damaged.
How We Handle
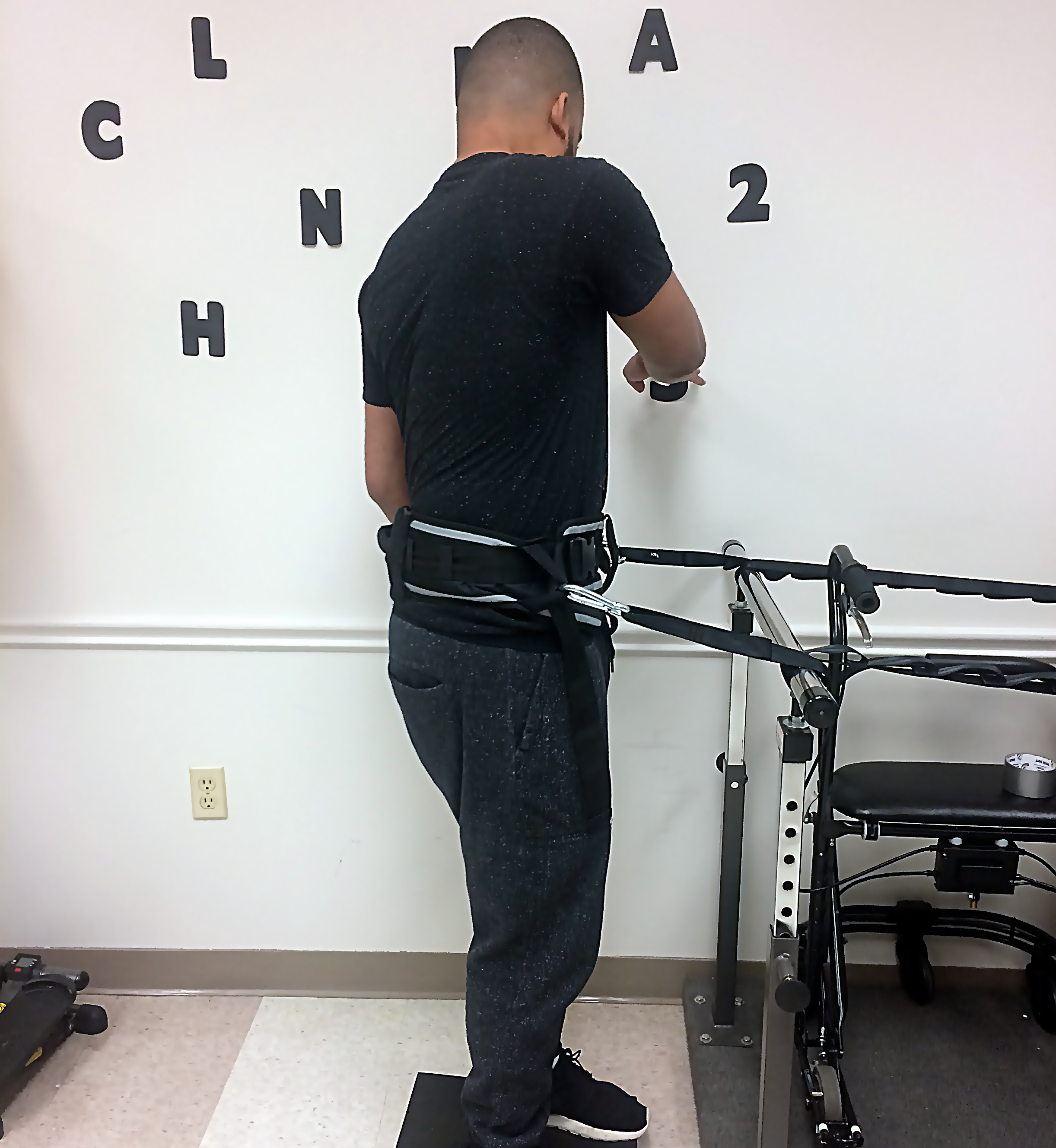
Brain Injury Rehabilitation
We understand the severity of a brain injury and the problems that it can cause in your life. That’s why our treatment approach focuses on restoring normal movement and regaining functional independence as quickly as possible. We do this with a serious focus on getting the most work done during your sessions. You’ll be seen exclusively by a board-certified specialist, never double booked, and we’ll never ask you to do unhelpful, monotonous exercises so that we can catch up on paperwork. Getting you back to a pain-free, independent life is our primary focus.
- One-on-One Patient Care
- Only Board Certified Specialists
- Less Paperwork – More Treatment
How We Handle
Brain Injury Rehabilitation
We understand the severity of a brain injury and the problems that it can cause in your life. That’s why our treatment approach focuses on restoring normal movement and regaining functional independence as quickly as possible. We do this with a serious focus on getting the most work done during your sessions. You’ll be seen exclusively by a board-certified specialist, never double booked, and we’ll never ask you to do unhelpful, monotonous exercises so that we can catch up on paperwork. Getting you back to a pain-free, independent life is our primary focus.
- One-on-One Patient Care
- Only Board Certified Specialists
- Less Paperwork – More Treatment
The Signs & Symptoms of a Brain Injury
A brain injury can occur anywhere in the brain. The resulting impairments from a brain injury will depend on where in the brain the damage occurs. The severity of the symptoms will also be different for each person.
The most common brain injury symptoms are
Thinking issues
Memory loss
Speaking issues
Vision loss
Upper/lower extremity weakness
Balance issues

The Signs & Symptoms of a Brain Injury
A brain injury can occur anywhere in the brain. The resulting impairments from a brain injury will depend on where in the brain the damage occurs. The severity of the symptoms will also be different for each person.
The most common brain injury symptoms are
Thinking issues
Memory loss
Speaking issues
Vision loss
Upper/lower extremity weakness
Balance issues
History and Background
A brain injury is the disruption or death of nerve cells in the brain. (1)This can occur from blunt force trauma (ie: those that occur in motor vehicle accidents, falls, and contact sports), a penetrating injury (ie: stabbing, and gunshot wounds), space occupying lesion (brain tumor), or from deprivation of oxygen to the brain leading to cell death (infection in the brain, heart attack). A brain injury can range in severity from mild to severe and effect vision, thinking and reasoning skills, memory, emotions, and motor function.
What is a brain injury classification?
Classifying the severity of a brain injury helps healthcare professionals establish an appropriate plan of care as well as help the health care community to communicate with eachother using a common language. The following are assessment tools commonly used for the above stated purposes.
The Glasgow Coma Scale (GCS) is a 15 point scale that looks at spontaneous eye opening, motor response and verbal response and is used in the first 48 hours following the brain insult. The score classifies the brain injury as mild (score 3-8), moderate (9-12) or severe (13-15).
The Rancho Los Amigos Scale of cognitive functioning is used during the recovery phase to define where the patient is in the recovery process. There are 8 levels.
- Level I: No response
- Level II: Generalizes Response
- Level III: Localized Response
- Level IV: Confused-Agitated
- Level V: Confused-Inappropriate
- Level VI: Confused-Appropriate
- Level VII: Automatic-Appropriate
- Level VIII: Purposeful-Appropriate
The Simplified Motor Score (SMS) is a 3 point scale that was developed for a more simplified scoring system.
- Obeys Commands = 2
- Localized Pain = 1
- Withdraws to pain or worse = 0
What Causes A Brain Injury?
Traumatic Brain Injury – Insult to the brain that occurs after birth from a mechanical external force causing damage to brain tissue. Cerebral hypoxia – Brain tissue can also be damaged with their is a loss of blood flow, depriving the brain of oxygen. There are is focal hypoxia (which occurs following an ischemic stroke and diffuse cerebral hypoxia.
Mechanism of Injury
A contusion occurs on the brain when either the head collides with a stationary object or the head is forced into high speed movement causing brain tissue to stretch or deform beyond the tensile or elastic capabilities of the brain tissue.
Coupe Contusion
When the head is struck by a small object, the force is over a smaller surface area and causes a contusion at the site of impact. This type of contusion is a coupe contusion.
Contrecoupe Contusion
When the head is struck by a larger object the brain is able to dissepate the force at the site of impact however the brain is forced into a rapid movment causing a collision with the opposite side of the skull. When the contusion occurs on the opposite side of the brain from the initial impact, this is call a contrecoupe contusion.
Secondary Brain Injury
Secondary brain injury is injury to the cells not related to the initial insult that may occur days or weeks following the initial injury.
Increased Intracranial Pressure (ICP)
An increase in pressure >40 mmhg following the injury can lead to further cell death
Cerebral Edema (brain swelling)
This can occur due to an increase in the ICP. Furthermore, several neurochemical processes are impaired resulting in disruption in the autoregulation of blood vessels to expand and contract appropriately.
Hydrocephalus
The insult can also disrupt the flow of cerebral spinal fluid (fluid that surrounds the brain to act as a cushion)
Brain Herniation
This can occur due to increase ICP or uncontrolled cerebral edema where the brain has expanded beyond the available space in the skull and brain tissue is forced our of a foremen (opening) in the skull.
Brain Injury Recovery
What you need to know in the acute phase (first 1-2 weeks) following a brain injury?
Depending on the severity of the brain damage, patients will stay in an intensive care unit where they for close monitoring.
Lines, tubes, and “noises”: In this stage the medical team monitors heart rate, ICP, blood oxygen saturation, breathing rate, and heart rhythm. Alarms are set up to quickly notify the nurses should any of these numbers make the slightest change.
Intravenous (IV) lines: Often times patients will have an IV line to quickly and easily administer medications, electrolytes, and fluids. The IV is extremely important. Therefore it is also common to see mits, boards, and soft splints to protect the IV from becoming dislodged
Nasal Gastric (NG) tube: Often times a tube will be inserted through the nose that lead to the stomach to maintain proper nutrition
Breathing Tubes: Patients may have a breathing tube. If an airway cannot be maintained through the mouth, this tube may be inserted through the neck (tracheostomy).
Medically Induced Coma: For a patient to recieve the propr medical care, a doctor may decide to keep the patient in a medically induced coma.
Visitation: Patient’s can often times hear. Having familiar voices in the room may bring a patient in this stage comfort.
Children: it is important to thoughtfully consider a childs age and maturity level before bringing them to this setting.
Progressive Care Unit (step down unit): Once the doctor is confident that all critical (life threatening) issues have been resolved, the patient is usually transferred to a step down unit. Many of the life sustaining lines and tubes that were present in the ICU will be taken off. Patients vitals are still monitored.
Brain Injury Rehabilitation
Inpatient Rehabilitation (weeks – months following the initial injury)
Often times patient’s will need to go to a rehabilitation facility where they will work on gaining more independence prior to going home. At this stage, patients are medically stable and often times continous monitoring of vitals is changed to intermittent monitoring. The goals for rehab is for pateints to gain independence for a successful transition back to home. Patients are encouraged to wear “street clothes”. Here the medical team will challenge the patient to perform bathing, dressing, grooming, and eat meals with as little help as possible.
Outpateint Rehabilitation (months – years following injury)
Once the patient is in the home environment, outpatient therapy will focus on higher level physical and cognitive training. This can last up to 2 years after the injury depending on the patients goals. At this stage the additional resources page may provide helpful links and information.
HEAR FROM OUR PATIENTS
“Tara is a great physical therapist. She thinks outside the box and is always inventing new ways to challenge my son and keep him progressing. She goes way above and beyond. We have been in many physical therapy environments over the years, and Tara has had the greatest impact on my son’s recovery. She has pushed him to new limits. He continues to improve and Tara continues to pour hope into him. He loves working with her and loves seeing the functional improvements in his life. We are so thankful for Tara’s practice and all she does for her patients”
“Tara is Awesome! She has helped my Mother stand and walk with assistance after having a major stroke last year. She is the most dedicated person in her profession. She is determined to see that her patients achieve the most they can and continue to strive to meet their goals. She has never given up hope for Mom and we don’t know what we would have done if we had not been introduced to her. Thank you so much Tara for your continued enthusiasm and support!”
My daughter suffered a severe hemorrhagic stroke in February, 2016. She received 6 weeks of inpatient therapy, as well as months of outpatient therapy. She, unfortunately, suffered several falls and broken bones, and also developed severe spasticity of the left foot/ankle. I found Tara on the website around December of 2017 and called her about my daughter. She evaluated her and immediately began a vigorous treatment plan. We, at this time, were becoming quite discouraged and looking for hope. Now, just 6 months latter, the progress my daughter has made is beyond anything we could have imagined at the time we met Tara. Every session Tara works extremely hard, is focused and uses a great bedside manner to elicit results from her patient. She shares the joys of her patient and their family when improvements are made, and she shows great pride in her skills. Tara is the best physical therapist we have had the privilege of working with. When we began with Tara, my daughter was confined to a wheelchair, she now is able to get that left foot flat and walk with assistance. Tara also helped us secure a new brace that actually works. Also, my daughter loves going to her therapy. sessions!
Contact us to start living a more confident, pain-free LIFE!
Call now to speak directly to a therapist

(407) 900-0841



